The airm of “Research Center for Sex- and Gender-Specific Medicine” in the Seoul National University Bundang Hospital” is to perform the comprehensive research in the variety of clinical areas in terms of Sex- and Gender-Specific Medicine to provide the basis for the precision medicine.
An interactive “Research Center for Sex- and Gender-Specific Medicine” will improve the ability of health researchers and students to consider sex and gender in the whole process of research, from research design, data collection, data analysis and application the results in all research models ranging from human participants, animals and cells. Finally the goal is the precision medicine and individualized medicine. Our research center is the first in South Korea and will respond the demands of Sex- and Gender-Specific Medicine and finally lead the Genered Innovation.
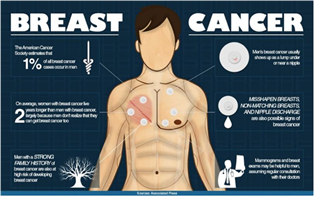
Medical researchers and clinicians recognize that it is important to understand differences related to age, for example between young and old people. Similarly, it is important to understand the physiological/physical differences among women, men, and non-binary people. The differences among women, men, and non-binary people can be divided into sex differences, which respond to hormones and genetic factors, and gender differences, which are related to differences in women’s and men’s distinct social and cultural roles. Importantly, these two aspects—sex and gender— interact and together influence health outcomes. Thus sex and gender are modifiers of health, disease, and medicine. Sex/gender-specific medicine refers to the health-related differences between women and men. Although many researchers and clinicians believe that sex differences are already well understood, experts point out that even where females and males are included in a study in equal numbers, data are often not disaggregated and analyzed by sex. As a result, medical studies tend to present an “average” for each disease - an average that may not accurately describe either females or males. This issue is very important because studies that fail to disaggregate and analyze data by sex miss specific disease mechanisms and treatments for women, men and non-binary people. For example, estrogen receptors (ERs) have widespread effects in numerous cells throughout the body, not just in reproductive organs. This means that differences between females and males in estrogen levels impact cells well beyond the reproductive system. In light of these findings, researchers have been actively investigating conditions where the disease incidence is higher in one sex, or where clinical manifestation are different between women and men even where the disease incidence is similar. Prominent examples include brain development, cardiovascular disease in women, osteoporosis in men, and stem cell research. Why is the “Research Center for Sex- and Gender-Specific Medicine” necessary? Ultimately, the reason is that research for sex/gender-specific medicine improves health outcomes. Women and men may suffer from different diseases; they may also present with different symptoms in the same disease. Biologically, these differences may be caused by the effects of sex hormones or genetic predispositions on disease mechanism (i.e., pathophysiology). Culturally, these differences may be traced to gender differences in social roles, attitudes, and behaviors, which may impact the incidence or expression of disease. Some prominent examples of sex and/or gender differences in disease include myocardial infarction, the clinical symptoms of heart failure, rheumatic disease, and autoimmune diseases. For instance, myocardial infarction and sudden ischemic death is more common in men, meaning that treatment is often delayed in women who may present with atypical symptoms, such as epigastric soreness or heaviness instead of pain in the chest. Since coronary syndromeqk related to stress is more common among women, exercise stress testing is less effective for women than for men. Differences are common in other diseases. The ratio of women to men among patients with rheumatoid arthritis is 2 to 3:1. Although there are no specific clinical differences, women tend to evaluate their pain as more severe than do men, meaning that disease activity is greater in women. In addition, women suffer comorbidities, such as depression, thyroid disorders, and fibromyalgia, while men suffer more cardiovascular diseases. Experts in these fields may be familiar with these differences but students, interns, and residents rarely are. Thorough familiarity with these differences can assist in diagnosis and treatment, underscoring the need for sex/gender-specific medicine. “Research Center for Sex- and Gender-Specific Medicine” will help the integrative research from basic science of animals and human beings to clinical areas. In addition, the experts of human science who can overview the whole humanities harmonize our research and raise the quality of Sex- and Gender-Specific Medicine. The mission is very clear but the roads to this vision could be tough.